Medical issues & health assessments
There are some condition that require referral and/or medical clearance in order to receive weight management counselling.
These conditions can have specific nutritional requirements different to other people.
Health assesments
Health screenings are required to assess your status and identify any special needs before starting a weight management program. Your doctor may request modifications to your plan to accommodate your specific medically necessary nutritional needs.
Medical clearance ensures:
- minimise the chances of the weight management program or product exacerbating a pre existing ailment or medical circumstance;
- gain professional medical input, where applicable, to enhance the chances of the weight management program or product benefiting a pre-existing ailment or medical circumstance.
Health assessments initially take place as part of the initial consultation process to identify areas of concern. Health screenings include:
- general health status
- presence of chronic disease, and
- medication use
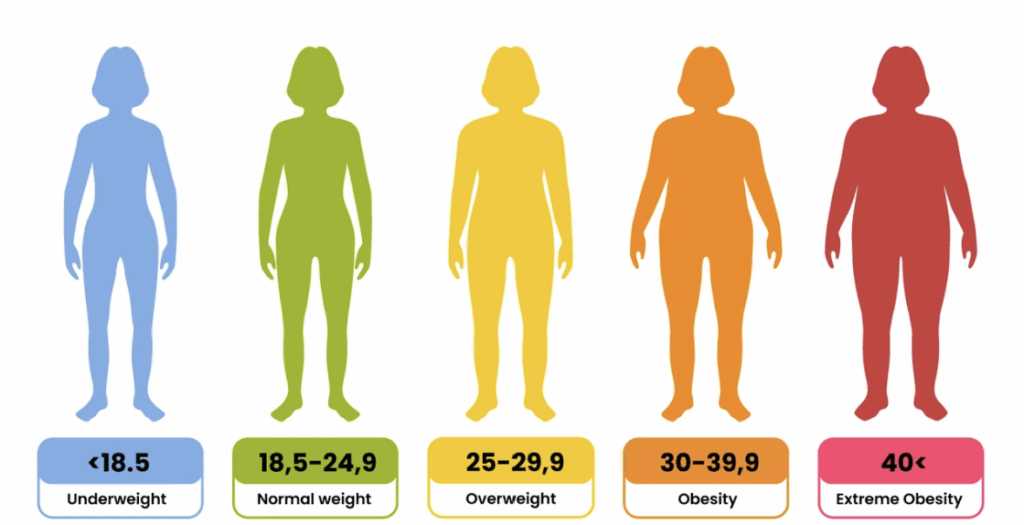
BMI
BMI is one way of assessing a clients weight status. While not foolproof as it does not take into account body composition (fat and muscle distribution), it gives a good general indication.
BMI is a tool that provides a number to indicate if a person is of a healthy BMI or not.
Other tools to assess weight status for health include Body fat scales, and waist circumference.
source: https://www.betterhealth.vic.gov.au/health/healthyliving/body-mass-index-bmi
Waist circumference
Waist circumference is a better indicator of health risk.
From Better Health:
For men:
- 94 cm or more – increased risk
- 102 cm or more – substantially increased risk.
For women:
- 80 cm or more – increased risk
- 88 cm or more – substantially increased risk.
When considering what this looks like think like this:
- least risk – slim (evenly distributed body fat)
- moderate risk – overweight with no pot belly
- moderate to high risk – slim with pot belly
- high risk – overweight with excess belly fat.
Medical conditions and nutritional requirements
Pregnancy
There are extra nutrient requirements when a person is pregnant. Nutrients of concern are: Folate, iron, calcium, vitamin D, protein and iodine1. There is very little additional energy requirement so a pregnant person should not eat for two2. There are also some foods that are unsafe to eat while pregnant. These foods include deli meats, soft cheese, large fish (due to mercury risk), some raw foods and many more. For a more comprehensive list, click here.
Referral and/or co-management with an obstetrician, specialist dietician and primary care provider is advisable.
Coeliac disease and malabsorption diseases
People with Coeliac disease need to be on a strict gluten-free diet for life. Along with other malabsorption diseases, malnutrition is a risk. Doctors may prescribe supplementation of nutrients where a person may be deficient due to malabsorption.
For a quick guide on Coeliac disease click here.
source: https://my.clevelandclinic.org/health/diseases/22722-malabsorption
Referral and/or co-management with an accredited dietician and primary care provider is advisable.
adolescent diabetes
Care should be taken to have regular and frequent meals through the day and lower GI foods are recommended. Hydration is especially important.
It is recommended to get support on individual diet requirements from a dietician.
Referral and/or co-management with an endocrinologist, an accredited dietician, a credentialed diabetes educator, and a primary care provider is advisable.
medications that contain: mono-amine oxidase inhibitors, lithium, anticoagulants
It is recommended to maintain a consistent vitamin K intake when taking anticoagulants.
A low Tyramine diet is recommended for those on mono-amine oxidase inhibitors (MAOI)
Those on lithium medications should avoid a low-sodium diet and ensure adequate hydration.
Referral and/or co-management with the client’s psychiatrist or prescribing doctor is indicated to manage any possible drug/diet interactions. An accredited dietitian is recommended to advise on foods to avoid.
eating disorder or a history of an eating disorder
Those recovering from eating disorders are recommended to base their diet on complex carbohydrates such as bread, pasta, rice and cereals. Regular eating and learning what normal eating is are recommended. All foods should be considered acceptable to avoid disordered eating.
Psychological may be recommended.
Referral and co-management is recommended with a qualified psychologist/counsellor specialising in eating disorders.
obese or overweight children (until they have completed puberty)
Special care should be taken regarding meal plans to support obese or overweight children. Weight loss can affect or delay the onset of puberty and affect growth. The Australian Dietary Guidelines recommend that children not be on a low-fat diet, but the focus should be on a balanced diet.
Referral and/or co-management with an accredited dietitian and primary care provider is advisable.
body mass index below twenty (20)
A BMI of under 20 indicates a person is likely to be underweight. Nutritional care would focus on healthy weight gain.
Depending on the cause of the low BMI, referral may be required to a psychologist/counsellor (in the case of eating disorders), or other specialist related to the cause. Being underweight may be caused by illness, and the primary care provider should be involved in co-management.
cancer
For those with cancer the recommendations are to abide by the Australian Dietary guidelines. Especially for its benefits in supporting immune function, healing and other health benefits.
Co-management is recommended with the client’s oncologist and primary care provider.
diabetes insulin-dependent
A balanced diet is recommended, with the suggestion that snacks between meals may be necessary. Low GI is also recommended.
Referral and co-management are recommended to an accredited dietitian and primary care provider.
epilepsy
Diet can improve seizure control for some people with epilepsy. Low-sugar and ketogenic diets are often recommended.
Referral and co-management are recommended with an accredited dietitian and the primary care provider.
gall bladder disorder or Stones
Fast weight loss should be avoided as this can increase the chances of stones. A balanced diet low in sugar and unhealthy fats is recommended.
Referral and co-management are recommended with an accredited dietitian and the primary care provider.
liver or kidney disease
The nutrition for liver or kidney disease can be complex, taking into account fluid retention and the interactions between the liver and the kidneys. Low sodium and moderating kidney function is recommended. Higher fat content in healthy fats is recommended to prevent weight loss.
In kidney disease, be wary of an imbalance.
- Sodium
- Potassium
- Phosphorus
- Calcium
- Protein
Referral and co-management is recommended with an accredited dietician and the primary care provider.
major surgery – three months post-operatively
Advice should be sought depending on the surgery performed. However, to aid healing, a diet rich in protein, iron and vitamin C is often advised. After recovery, a balanced, healthy diet is recommended.
Referral and co-management may be recommended with the primary care provider.
breast feeding
There are extra nutrient requirements while breastfeeding. Ensure you eat a balanced diet, with a special focus on obtaining adequate levels of protein, calcium, iron, iodine, vitamin D , and other essential vitamins.
Referral and co-management may be recommended with an accredited dietitian and the primary care provider.
gout
Care should be taken to avoid foods high in purines, which can lead to a buildup of uric acid. This includes many meats, shellfish, high fructose foods and alcohol.
Referral and co-management are recommended with an accredited dietitian and the primary care provider.
gastro intestinal disease
A balanced diet is recommended where it is tolerated. Depending on the severity, a dietitian should be consulted.
Referral and co-management are recommended with an accredited dietitian and the primary care provider.
medications – e.g. steroids
Consult with your GP regarding the nutritional changes required for your prescribed medications. Advice will vary depending on the medication.
Referral and co-management are recommended with an accredited dietitian and the primary care provider.
thyroid disease
A balanced diet is recommended for thyroid disease. Some foods may be an issue, and some may have an effect when paired with thyroid medications (timing of these foods is advised). They include brassicas (broccoli, kale, cabbage, etc), kelp (and iodine supplements), soya, and calcium-rich food.
Referral and co-management is recommended with an accredited dietitian, endocrinologist and the primary care provider.
chest pain (undiagnosed) or severe shortness of breath
The cause of chest pain should be investigated with your primary care provider, and nutrition should be guided by any relevant diagnosis.
Referral and co-management may be recommended depending on the diagnosis.
angina
A balanced, healthy diet is recommended, especially as angina can be caused by coronary heart disease, which can be partly caused by poor diet choices.
Referral and co-management are recommended with a cardiologist, an accredited dietitian and the primary care provider.
cardiac arrhythmia
Heart-healthy diets are recommended. The avoidance of aggravating foods is recommended: caffeine, alcohol, tyramine, sodium and oversized portions.
Referral and co-management are recommended with a cardiologist, an accredited dietitian and the primary care provider.
heart disease/heart attack/coronary bypass surgery
food allergies or sensitivities
in consultation with an allergist, immunologist and dietician, care should be taken to address allergies and find nutritional substitutions to foods that cause severe allergic reactions.
Along with the above referrals, co-management with the primary care provider is recommended.
concurrent medically prescribed diet for health problems
When the client is on a specified diet due to health problems, it is advisable to discuss any nutritional plan for weight management with the prescribing doctor.
Co-management is recommended with the prescribing accredited dietitian and the primary care provider.
physical limitations that may reduce exercising capacity
Depending on the cause or type of physical limitation, nutritional needs will vary. If a person’s ability to exercise is reduced, their calorie requirement may be lower. However, it is also possible that a person’s disability may require additional nutrients.
Referral and co-management are recommended with a physiotherapist/exercise physiologist and the primary care provider.
arthritis on medication
Avoiding unhealthy fats can help alleviate symptoms of arthritis. Aiming to reduce weight when overweight is also recommended.
Referral and co-management are recommended with a rheumatologist, an accredited dietitian and the primary care provider.
controlled depression
A balanced diet supports reducing mental health symptoms of depression. Awareness of mindful eating habits could mitigate the issues of under- or overeating in this group.
Referral and co-management are recommended with the client’s psychologist/psychiatrist/counsellor, and the primary care provider.
type II Diabetes only where insulin is not part of the therapy
A balanced diet and nutrition to support weight loss (where indicated) support health improvements for people with diabetes. Low GI foods are recommended.
Referral and co-management are recommended with an endocrinologist, an accredited dietitian and the primary care provider.
high blood pressure or high blood cholesterol.
The DASH diet is commonly recommended for people with this medical issue. It is low in salt and saturated fat and is based on fruits, vegetables, grains, fish, poultry, beans and nuts.
Referral and co-management are recommended with a cardiologist, an accredited dietitian and the primary care provider.
References
- https://www.thewomens.org.au/health-information/pregnancy-and-birth/a-healthy-pregnancy/food-nutrition-in-pregnancy
- https://www.eatforhealth.gov.au/eating-well/healthy-eating-throughout-all-life/healthy-eating-when-you%27re-pregnant-or-breastfeeding